From artificial intelligence to lab-grown organs, the development of new technology to save lives and make people healthier has never been so exciting, writes Pádraig Belton. And from start-ups to universities and big hospitals, Ireland is in the forefront. So here are 23 new technologies to watch, which will be changing healthcare forever in 2023

1. Growing organs in Dublin and Galway
“We have lots of cool bioinnovation in Ireland. It’s great to see them get some attention,” says Dr Laura Durcan, pictured above, a consultant in rheumatology and internal medicine at Beaumont Hospital. Niall Davis, a consultant urologist at Beaumont, has received patents for “regrowing bladder cells that have been removed by cancer,” she says.
And in Galway, Bioinnovate alum Dr Brendan Boland has got investors’ thumbs up for his Loci Orthopaedics start-up, manufacturing a prosthetic surgical replacement for a thumb base joint he calls “one of the most remarkably complex but beautifully elegant joints in the body” and which is also the third most common joint affected by arthritis.
His start-up received €8.1million in funding in 2022.
2. Not just a phage > fixing antibiotic resistance
In big-scale medical terms, the world’s “biggest problem is antibiotic resistance,” says Joanna Potter, a lecturer at University College Dublin. So given “we already have vast colonies of resistant bugs in various places” looking for possible solutions looks pretty high on the medical to-do list.
Antibiotic overuse just selects for strains of microbes that antibiotics can’t kill. But providing one possible alternative to antibiotics, microbiologists are developing bacteriophages, a type of virus that targets bacteria.
One of these, PSD9, produces a lytic enzyme P9ly that can destroy Shigella – a highly transmissible bacteria with strains that are extensively drug resistant. Another new approach is using the vibration caused by bacterial cells to provide information about which antibiotic should be used to treat a particular patient. Resistell says by using this approach, its diagnostic device can reduce the time to get a result from days to hours.
“This one will change the game and is one of best funded Swiss startups in the field,” notes Dr Aleksandar Petrovic, a senior global medtech principal at Iqvia in Basel. Meanwhile, using synthetic meat and plant-based protein sources will “take out the middle animal, therefore less antibiotic use in the food chain”, offers Potter.

3. Virtual wards
Twin brothers David and Thomas Coleman, pictured above and based between Dublin and Enniskillen, founded a company called Zendra Health to help healthcare services easily create virtual wards using tech.
These virtual wards, which can let patients monitor their oxygen levels from home “were at the fringe until the Covid-19 pandemic occurred” but after 2020 “became a crucial tool” – helping free up staff and beds and mitigate the surge in demand on hospitals, says Thomas Coleman, pictured with his brother David.
While patients enjoy their time within the comfort of their own homes, wearable devices collect their vital signs and these are then monitored by clinicians through a secure dashboard.
Continuing to roll out and expand virtual wards is one of the top priorities for the NHS in 2023, he says. Virtual wards are like ‘mission control centres’ where clinicians can look after patients who otherwise would have been at hospital taking up bed capacity, or in the community worrying about their health, explains Martin Ratz, founder of Doccla, another virtual ward company.
Post pandemic, these have expanded into the mainstream, growing from acute respiratory infections to helping patients with other conditions, such as frailty, cardiovascular disease and mental health diagnoses, to be treated at home.

4. Wearables to treat wounds
Based in An Spidéal in Connemara, Dr Andrew Cameron’s start-up FeelTect is working on using wearable technology, digital platforms and data-driven insights to make life better for people living with open sources.
Venous leg ulcers, which often affect the elderly, can have enormous impacts on their quality of life, says Dr Cameron. Compression bandages are the “first line” of treatment, he says, but people bandaging their own wounds often have trouble applying their bandages correctly.
Tight Alright, Dr Cameron’s connected-health platform for bandages, tells people when they’ve tied their bandages with a level of
pressure that is safe, effective and will reduce their healing times.
This reduces workloads for nurses, helps people manage their own conditions, while letting clinicians remotely monitor their recovery and tailor their treatment. He says he hopes to “develop a pipeline of technologies” in coming years to monitor wound treatment.

Picture: Bríd O’Donovan
5. Gift of the Gabadoo
Speech and language therapy is vital to the people it can help, but has huge waiting lists, as does occupational therapy. Both are areas where demand grows every year, but there has been little innovation over the last two decades.
So one Irish start-up has come up with an asynchronous telehealth model to connect these services faster with families who need them.
Technology has “allowed us to scale what was typically seen as unscalable,” says Seán Ó Tuama, co-founder of Gabadoo, which recently won the Tech4Good prize in the Technology Ireland Industry Awards.
“We have cut waiting times to access these supports from years to just hours,” says Ó Tuama, pictured above with co-founder and CCO Jessica Kennedy. Over 70 therapists across Ireland and the UK have onboarded Gabadoo so far.
6. Get me to the GP on time
Martina Skelly, founder of Limerick-based YellowSchedule, had a big motivation to start her start-up – one that makes specialist software for healthcare scheduling. It came out of her own frustration with missing a medical appointment for one of her children.
Digital tools can gather information from patients when they book their appointments, to direct them to a more relevant clinical professional, and thus increase patient access while also slashing waiting list bottlenecks.
“Waiting months to see an orthopaedic consultant, only to be referred to a physiotherapist at the first appointment, is not an efficient use of time for anyone,” she says.
7. Computational cancer treatment + making personalised medicine accessible
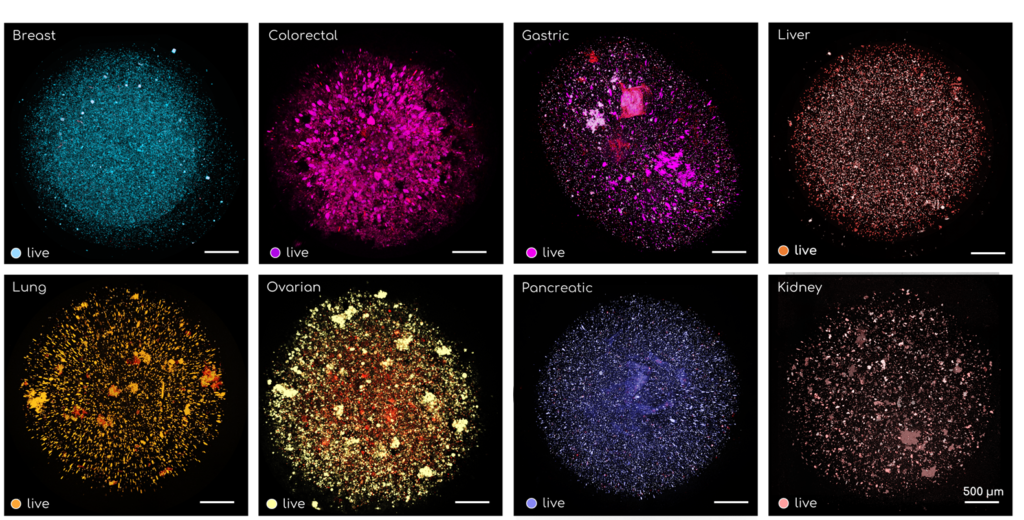
Meanwhile recent UCD graduate Steven O’Connell, operations lead at start-up Pear Bio, is using computational biology and “organ on a chip models” to recommend drugs likely to work for a particular cancer patient.
This platform uses tumour samples and 3D computer vision to test potential different treatment options. The 3D microscopy data yields information about particular biomarkers in the tumour, and then AI algorithms can suggest different alternative treatments that will be most effective for those biomarkers.
Personalised cell and gene therapies are the “first truly curative” cancer treatments, says Luc Henry, head of Limula, a Swiss start-up. But these ‘living drugs”, as he calls them, will only revolutionise healthcare “if they can be made in large enough quantities to reach the millions of patients in need”.
So performing all the steps of making a personalised cancer drug in a single device – and Limula has created one – can make the process more scalable, and safer. Automating steps that are currently done manually will make personalised cell and gene therapies “more broadly accessible”, he says.

8. Gender affirmation surgery
Dr Sidhbh Gallagher, a UCD graduate and plastic surgeon who has begun a plastic surgery practice in Miami working with her sister Neasa, “does very frontier stuff on gender affirmation surgery,” notes Beaumont Hospital consultant Dr Laura Durcan. The Irish surgeon, pictured, changing lives for transgender Americans has acquired a massive social media following of 270,000 on TikTok.
She opened a clinic in 2020, after five years as assistant professor of surgery at the Indiana University School of Medicine, where she started a Gender Affirmation Surgery Programme.
It’s also a route that, while developing new surgicaltechniques, has required personal bravery. Agents from the US Federal Bureau of Investigation contacted Dr Gallagher last year to say they had picked up “online chatter” about a plot to target her clinic. “She’s from Louth and very cool,” Dr Durcan says.

9. Holographic patients
Maybe you’ve learnt CPR on a legless plastic mannequin – maybe even a St John Ambulance ‘Annie’, or something like it. An actual patient in cardiac arrest (hopefully) looks a bit different.
Real-world cardiac arrest is noisy and confusing, with gathered crowds panicking or attempting to help. Hyper-interactive, immersive 3D can let both medical professionals and community first aiders interact with more realistic patients, in more real-world scenarios.
And if you have a headset and internet, you can train with the holographic simulator from anywhere in the world. Immersive reality company GigXR has worked with medical simulation experts at Morlen Health, a subsidiary of Northwest Permanente, to create just such an application, which they call HoloScenarios.
“Mixed reality is the future of medical education,” says Dr Patricia Ramos, senior emergency physician at Kaiser Permanente Northwest and the start-up’s medical director.
10. Listening to your gut
On the quirkier side, London-based Biomesight has been exploring what machine learning models can discover about a person from sequencing the DNA in their gastrointestinal tract. And what health insights can come from this, notably in tweaking your diet.
“We’ve achieved over 90 per cent accuracy in predicting whether a sample is from someone with long covid, which is a major accomplishment,” says Rose Walbrugh, its founder.
The diversity of your gut microbes has been linked to everything from depression to how people respond to cancer treatments. The start-up uses a lab in California to sequence the 1,500 base pairs in the 16S rRNA gene in gut bacteria. This is a small subunit that appears in distinctive ways in all bacteria, and can be used as a fingerprint.
And how can you get to all this ecosystem you host in your gastrointestinal tract? Well, in the name of a book by Professor Felice Jacka, a nutritional psychiatrist and director of the Food and Mood Centre at Deakin University: There’s a Zoo in My Poo.

11. Using glycans to spot cancer and other diseases early
Compounds called glycans “are a measure of immune ageing and change up to a decade before cardiovascular disease, diabetes, and many other inflammatory conditions,” says Nikolina Lauc, founder of London-based GlycanAge, pictured above.
Her start-up, she says, can measure changes in these chemicals and make “prevention a realistic option”. Others working in the same field include San Francisco’s InterVenn, which works on detecting cancers (especially ovarian cancer) accurately and early through glycobiology.
And GlycoScore, a UK start-up which focuses on detecting prostate cancer accurately and early through glycobiology – and in 2021 raised £1million in seed funding. Their technology can detect the presence of prostate cancer with an AUC (area under the curve, the probability of telling two things apart correctly) of 0.94, while “the current gold standard is 0.60,” says Lauc.

12. Women’s reproductive health
Research into novel contraceptives “might be able to preserve fertility and delay menopause,” says Nikolina Lauc, founder of London-based GlycanAge. And by expanding women’s reproductive timelines to that of men, this “would make a more equitable world,” she says.
One spinout which is working on just this is Oviva Therapeutics in New York, headed by Harvard-trained molecular biologist Daisy Robinton.
Her co-founder, Massachusetts General Hospital’s legendary Professor Patricia Donahoe, is an expert on the anti-Müllerian hormone (AMH), which she says can slow down the process by which the ovaries run out of eggs.
And delaying menopause by doing this will have huge impacts “on the reproductive health of women from all walks of life whose reproductive rights are currently under siege,” she says.
Another is London-based Dama Health, whose founder writes “the contraception crisis is real,” noting eight out of 10 women suffer from side effects of contraception and contraceptives “are commonly prescribed in a fast, inaccurate, and non-personalised manner.”
This largely happens because consultations with doctors are “too short to find the right fit”. Its technology therefore works on personalising contraceptive decisions based on a woman’s unique biology, to minimise side effects.

13. Equalising precision medicine
As precision medicine takes off more, there’s the problem that much of the world – like African genomic data, for instance – is under represented in research.
In summer of 2020, a 63-year-old black American woman with colon cancer began treatment with a common chemotherapy agent, fluoropyrimidines. But she had to be rushed into intensive care.
Like 20 to 30 per cent of the people who begin fluoropyrimidine treatment, she needed a lower dose, for reasons thought to be genetic. The gene involved in metabolising fluoropyrimidines was sequenced and studied before determining the right chemotherapy doses but these studies were only done on individuals of European ancestry.
So it will be important to close this “genomic gap”, and “equalise precision medicine”, by taking steps to make sure it’s not only the genes of people in the world’s wealthiest countries that are being studied, says Nikolina Lauc.
One Washington and Lagos-based company, 54gene, founded in 2019, has aimed to address this gap in global genomics, and landed several successful funding rounds. But the company saw jobs slashed and its CEO Dr Abasi Ene-Obong leave at the end of 2022.
For an indication of the sheer scale of the problem: one Nature paper in 2021 calculated three million African genomes need to be sequenced just to fully capture the continent’s genetic diversity.
14. Nutritious delicious and high tech too
Another take on using DNA sequencing to come up with personalised health advice is being explored by ZOE, a London and Boston based startup whose popular Covid-19 reporting app went viral (if that’s the word) in 2020.
Post Covid, Jonathan Wolf’s company has attracted a third funding round (and $250million valuation) by offering “precision nutrition” advice based on your unique biology: a gut microbiome test, a blood fat test and real-time blood sugar sensor.
The promise is that using cheap DNA sequencing and AI can help people find their way to sustainable weight loss and longterm health improvement.

15. Epilepsy and tech
About 75-80 million people in the world have epilepsy, which is also found “way more in lower-middle income countries,” says Torie Robinson, host of Epilepsy Sparks, a science podcast about epilepsy (which she also has).
In countries where access to healthcare is more limited than in Ireland or the UK, new phone apps and remote EEG recording
devices now increasingly let patients communicate with their clinicians remotely, and even have their seizures recorded.
This “significantly improves quality of life – for both the patients and families,” says Robinson, pictured above. Algorithms are
improving for diagnosis and care, too.
Other tech innovations for treating epilepsy, she says, include using graphene which enables doctors to “delve deeper into the brain to identify over the top activity”, she adds.
This is being studied by Dr Rob Wykes at UCL, and start-ups like Byteflies and UNEEG, developing devices where you place electrodes behind your ear, connect them to your smartphone and “record neuro data that would never otherwise be available to a clinician, and leads to far improved treatment that can save lives”.

16. Gene editing drugs
The first CRISPR gene-editing drug, to treat blood disorders, could enter the market in 2023. This is tech that won scientists Jennifer Doudna and Emmanuelle Charpientier the 2020 Nobel Prize in chemistry – using molecular scissors to snip away problematic bits of a patient’s DNA, and thus cure diseases.
It’s a development “I think is going to reinvent precision medicine,” wagers Arshia Gratiot, pictured above, London-based founder of Eupnoos, a start-up that uses smartphones and AI to test lung function.
Rare inherited blood disorders like sickle cell disease and beta thalassemia are likely to be among the first to benefit from gene-editing drugs.
CRISPR Therapeutics is working with rare disease specialist Vertex, to devise a new therapy called exa-cel (short for the somewhat more ponderous “exagamglogene autotemcel”),which has performed well in drug trials.
The drug could receive regulatory approval in Europe, the UK and the US by the end of this year.

17. Waking the sleeping pills
Chronic insomnia affects between 6 and 12 per cent of the population of Europe. But sleeping pills haven’t changed in 20 years, says Mark Chataway, Wexford-based co-owner of Hyderus, a medical communications firm.
Daridorexant, designed for people with serious long-term insomnia, “works by stopping you feeling always awake, rather than making you feel groggy”.
It does this by blocking receptors for orexin, a hormone that makes you feel awake. The drug, which doesn’t generate tolerance and had already been approved in the US, received European approval in May 2022. Sleep problems generally, though, represent a serious epidemic, which will be getting lots of attention in 2023 and beyond.
And sleeplessness is shortening lives. Life expectancy was 4.7 years higher for men and 2.4 for women for people who met all five of the sleep measures, compared to people who met just one or none of the criteria on the list, in a February study by the Harvard Medical School’s Dr Frank Qian.

18. AI and … leprosy
A new AI-driven diagnostic tool can identify leprosy before most humans can, with over 90 per cent accuracy. This tool, AI4leprosy, will have the effect of “making treatment easier and stopping the deformities seen in advanced cases,” says Mark Chataway, Wexford based co-owner of Hyderus.
Over 200,000 new patients are diagnosed with leprosy each year, and detecting and treating the disease early means being able to halt transmission and prevent the neurological damage that causes irreversible disabilities.
AI4leprosy was developed by an international team of scientists, from Brazil’s Instituto Oswaldo Cruz, Microsoft’s AI for Health team, and the Basel-basd Novartis Foundation.
19. AI and … scanning lesions
Artificial Intelligence is fast establishing itself in the field of dermatology. It holds out the promise of relieving pressure on the health service while expanding patient care, especially in important tasks like screening for the most dangerous skin cancers like melanoma.
A study in Nature showed an AI system produced by Google, interpreting photographs of lesions from a user’s smartphone using a machine learning model, was as good as a dermatologist at identifying 26 skin conditions.
Others working in the field include Skinive MD, and Skin Analytics (whose tool is called the Deep Ensemble for the Recognition of Malignancy, DERM).
Skin Analytics received UK approval for DERM in 2022 as a class IIa medical device.The Shoreditch-based company says its machine learning neural network is different from the others, being designed from the ground up for the specific problem of telling malignant, pre-malignant and benign skin lesions apart.
20. AI and … clinical trials
The coronavirus pandemic showed some of the limits of randomised controlled trials. They can often be slow, costly, inflexible and usually exclude elderly or infirm patients – making their conclusions generally invalid for those populations.
But it turns out, using machine learning to enhance clinical trials can reduce error and achieve greater confidence while requiring fewer participants. Traditional RCTs just allocate patients to treatment and control groups through uniform randomisation.
ML enhanced trials, like those developed by the Cambridge Centre for AI in Medicine, take a fundamentally different approach. These instead observe the treatment effects on each cohort before deciding who in the subsequent cohort should be assigned to the treatment or control groups, which speeds up learning.
“The biggest thing, as with the rest of the world, is going to be AI, and the Cambridge centre is doing amazing work,” says Gordon Gregory, a general surgeon and senior clinical fellow with the Cambridge University Hospital’s NHS Trust.

21. All eyes on AI from Ukraine
The war in Ukraine has seen a new health tech start-up develop a powerful AI-powered, cloud-based technology to detect diabetic retinopathy (DR): damage caused by diabetes and high blood sugar levels to the back of the eye, causing loss of vision and blindness.
It is an example of innovative medical tech coming “from the war zone”, says Dr Aleksandar Petrovic, a senior global medtech principal at Iqvia in Basel. Of the 6.5 million people internally displaced by Russia’s invasion of Ukraine, 29 per cent say they cannot access medicine and health services.
Hospitals are flooded with patients with traumatic injuries, and primary healthcare for conditions like diabetes strains under the pressure of mass migration.
Hence, Check Eye, and its AI-powered mobile DR screening. The plan is to offer free screening to at least 20,000 people with a pre existing diabetes diagnosis, in the three regions of Ukraine hosting the most internally displaced persons.
Ukraine “may end up with tens of thousands of disabled people among the working population if measures are not taken immediately,” says Kyrylo Goncharuk, the start-up’s chief executive.

22. Ear rings
Two doctors, Edmund Farrar and George Leidig, both developed tinnitus – ringing in the ears – in their mid twenties. Both as sufferers, and as doctors who had spent time working in the UK forces and in the NHS, they learned waiting lists for treatment on the NHS can be years long for this condition that affects one in every eight people.
So their solution was to offer a way to access cognitive behavioural therapy online, to help sufferers manage and live with the condition – combined with additional support by telehealth.
Oto, the London-based start-up which launched its product in 2021, helps 86 per cent of its users experience benefits after just one month. It’s also a prime example of technology helping healthcare become more efficient, by helping patients faster than health services can see them.
23. Magneto fixes your blood
Zurich-based Hemotune does dialysis, except for the bloodstream, which Iqvia’s Dr Aleksandar Petrovic calls “a remarkably novel idea”. The process works by attaching magnetic binders – with an ultra-magnetic core, combined with “affinity binders” that only attach to desired compounds – in a highly specific way to targeted impurities in a person’s blood.
Then, you take out a bit of a person’s blood, use a magnet to draw these impurities out noninvasively, reintroduce the blood … and repeat.
Last year, Hemotune raised 7.25 million Swiss francs (€7.29million) in series B1 investment for its blood purification technology, which can remove bacterial toxins from a person’s blood and is able to treat sepsis.
“This has the potential to do wonders,” says Dr Petrovic.






